Top Stories
Understanding Antibiotic Resistance: A Growing Global Crisis

The emergence of antibiotic resistance represents a significant global health challenge. This phenomenon is not new but has evolved alongside antibiotics themselves, which have been part of the natural world for hundreds of millions of years. Antibiotics are primarily produced by fungi and certain bacteria as a defense mechanism. As a result, the resistance of bacteria to these drugs has developed over time, reflecting the ongoing co-evolution between microorganisms and their environments.
In 1928, when Alexander Fleming discovered penicillin at St. Mary’s Hospital in London, it sparked a revolution in medicine. This breakthrough led to a wave of optimism among doctors and researchers who believed that bacterial infections could soon become a relic of the past. However, Fleming himself issued a cautionary note during his Nobel Prize acceptance speech in 1945, warning that improper use of penicillin could lead to resistance. His advice was largely forgotten as the period from 1940 to 1960 marked what is often referred to as the “golden age” of antibiotics.
In retrospect, this era came at a high cost. The widespread and often indiscriminate use of antibiotics not only nurtured our overconfidence but also contributed to the emergence of resistant bacterial strains. Today, healthcare professionals increasingly encounter bacteria that are resistant to all available antibiotics, creating a dire situation where effective treatments are scarce. Professor Gordana Mijović, an advisor to the Ministry of Health on antimicrobial resistance, notes that physicians often fear encountering patients infected with such resistant strains.
The question arises: how did antibiotics, intended to eradicate bacteria, contribute to their resistance? This may seem counterintuitive but is well explained by biological principles. Research has identified antibiotic-resistant bacteria even in remote regions of the Arctic and Antarctic, where human contact is minimal. In any population of bacteria that is generally sensitive to a specific antibiotic, some individuals will invariably carry mutations that confer resistance.
These resistant bacteria, while generally less competitive than their sensitive counterparts, can thrive when antibiotics are introduced. The treatment wipes out the majority of the population, leaving resistant strains without competition. As these resistant bacteria multiply, they can lead to infections that are difficult to treat, placing significant pressure on healthcare systems.
Recent studies have revealed concerning findings, including the presence of antibiotic resistance genes in bacterial samples stored in laboratories for over ten years. This indicates that resistant strains might exist globally, potentially against antibiotics that have yet to be discovered or utilized. The rate at which these resistant strains proliferate depends largely on the frequency and volume of antibiotic use that suppresses sensitive bacteria.
The “golden age” of antibiotics has thus led to an explosion of resistance. The silver lining, however, is that the process of resistance can be reversible. If the use of antibiotics is curtailed, sensitive bacterial populations can rebound, re-establishing control over resistant strains.
To combat antibiotic resistance effectively, a strategic approach is critical. This involves rationalizing antibiotic use, ensuring that these medications are prescribed only when necessary and for the appropriate duration. Scandinavian countries have successfully implemented such policies for over three decades, resulting in lower rates of resistance.
Current research is focused on determining the minimal effective duration of antibiotic therapies, with some protocols already significantly shortening treatment times. In some cases, infections can now be treated with one-day, three-day, or five-day antibiotic regimens, while others may still require longer treatments.
Rational antibiotic use entails adhering strictly to prescriptions, taking medications at the dosage and duration specified by healthcare providers. Failure to discipline ourselves in this regard could jeopardize our ability to effectively manage infections in the future.
The responsibility to address antibiotic resistance lies with each of us. Acknowledging this challenge is the first step towards safeguarding public health and ensuring that effective treatments remain available for generations to come.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science2 months ago
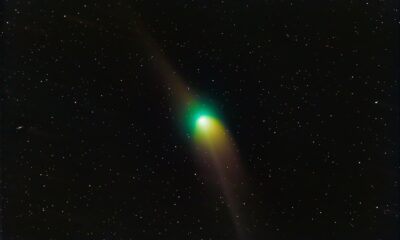
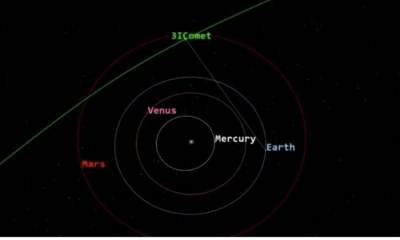
Science2 months agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science2 months ago
Science2 months agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science1 month ago
Science1 month agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment5 months ago
Entertainment5 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science1 month ago
Science1 month agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-

 Entertainment2 months ago
Entertainment2 months agoLewis Cope Addresses Accusations of Dance Training Advantage
-
 Science1 month ago
Science1 month agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-
 Entertainment4 months ago
Entertainment4 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









