Health
NHS Drug Pricing Needs Reform to Enhance Patient Access

Polly Toynbee’s recent characterization of NHS drug pricing as a “special circle of hell” highlights ongoing challenges in the United Kingdom’s healthcare system. While many agree with this assessment, there are viable solutions to improve the current drug pricing structure within the National Health Service (NHS).
Newly licensed medications tend to come at a higher cost than those they replace. Consequently, for the NHS to incorporate these new drugs, they must demonstrate substantial improvements in patient care. The majority of recently approved drugs provide significant benefits to various patient groups. Although some represent groundbreaking advancements, many offer incremental enhancements in the quality and longevity of life. The National Institute for Health and Care Excellence (NICE) typically recommends most of these new treatments.
Spending on new drugs inevitably diverts resources from other areas of the NHS. To navigate this financial landscape, NICE employs health economics principles to determine the most effective allocation of funds. Companies in the pharmaceutical sector often express concern that NICE’s value-for-money formula has not been updated for over 25 years. Despite this, NICE adjusts its baseline threshold to facilitate access to promising new treatments when necessary.
After receiving recommendations from NICE, pharmaceutical companies encounter additional hurdles. The NHS’s adoption of new medications can be slow, and when new drugs are introduced, there exists a negotiated mechanism between the pharmaceutical industry and the government that caps potential profits for these drugs.
Proposed Reforms to Drug Pricing
To enhance the drug pricing process, three key reforms are suggested. First, NICE and the government should establish an independent review of the value-for-money threshold and implement the resulting recommendations. This approach could lead to a more contemporary and effective assessment of drug pricing.
Second, NICE should establish specific take-up rates for the drugs it endorses. These rates would dictate the number of patients prescribed each year, and the NHS should commit to meeting these targets. This accountability could ensure that effective new treatments reach the patients who need them most.
Lastly, pharmaceutical companies should engage with NICE early in the pricing discussions. By presenting a realistic price from the outset, companies can avoid the pitfalls of negotiations that lead to price reductions after initial rejections. In exchange for this proactive engagement, companies would benefit from a special arrangement regarding the price cap.
These recommendations, proposed by Andrew Dillon, former founding chief executive of NICE from 1999 to 2020, aim to streamline the complex drug pricing process and ultimately improve patient access to essential medications. Implementing these changes could foster a more efficient and equitable healthcare system, benefiting both patients and the NHS alike.
-

 Health2 months ago
Health2 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health2 months ago
Health2 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science2 weeks ago
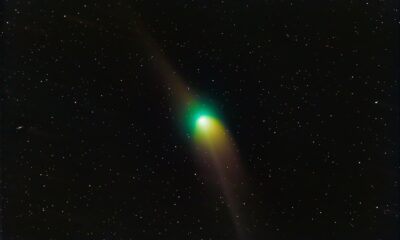
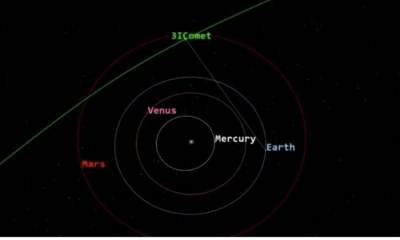
Science2 weeks agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science2 weeks ago
Science2 weeks agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science2 weeks ago
Science2 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science1 week ago
Science1 week agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 World2 months ago
World2 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-

 Entertainment3 months ago
Entertainment3 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-
 Science1 week ago
Science1 week agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment2 months ago
Entertainment2 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









