Health
B.C. Sees 49% Surge in Long-Acting Contraception Uptake

Following the decision to make prescription contraception free, British Columbia has experienced a significant increase in the uptake of long-acting reversible contraception (LARC). In just 15 months after implementing universal, no-cost coverage in April 2023, more than 11,000 women opted for LARC methods, representing a remarkable 49-percent increase in dispensations. This shift highlights a transformative change in how reproductive-aged women are managing their reproductive choices, according to new research from the University of British Columbia (UBC) and its collaborators.
Impact of Cost-Free Access
The study tracked nearly 860,000 women aged 15 to 49 and concluded that financial barriers had previously impeded access to effective birth control methods. LARC options, including intrauterine devices (IUDs) and implants, can cost up to $450 out of pocket, making them unaffordable for many. By eliminating these costs, British Columbia has provided a straightforward solution to enhance reproductive autonomy and prevent unintended pregnancies.
Notably, the policy’s implementation did not rely on extensive advertising campaigns. Instead, it was promoted through standard government announcements emphasizing the key message: “You won’t pay a cent.” This simple promise proved sufficient to encourage thousands of women who had previously been priced out of effective contraception to reconsider their options.
A Model for Broader Change
The implications of this policy extend beyond British Columbia, as it presents a compelling case for similar initiatives in other provinces and at the national level. Dr. Laura Schummers, the lead author of the research and assistant professor in UBC’s faculty of pharmaceutical sciences, emphasizes that the province’s success could serve as a blueprint for implementing national pharmacare. The clear evidence that cost-free access drives the uptake of the most effective contraception strengthens the argument for scaling up these initiatives.
“This could be a model for other provinces and for national pharmacare,” said Dr. Schummers. “By removing the cost barrier, we can facilitate access to the most effective contraceptive methods.”
The findings from this study will be published in the BMJ, underlining the importance of accessible reproductive healthcare. The increase in LARC usage not only reflects a change in individual choices but also signals a significant shift in public health policy that prioritizes reproductive rights and health equity.
As other regions look to improve their reproductive health services, British Columbia’s approach illustrates the significant impact that financial accessibility can have on healthcare choices. With a stronger case for expanding cost-free contraception, the province may well be leading the way toward a more inclusive healthcare system.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science1 month ago
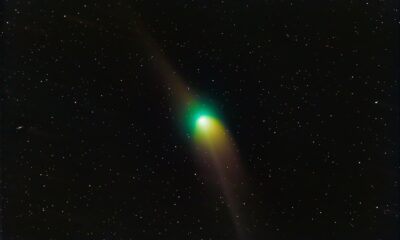
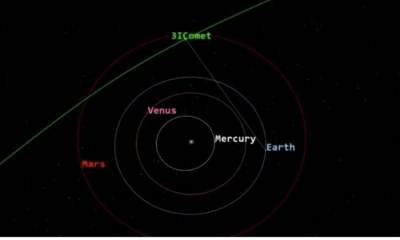
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science1 month ago
Science1 month agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science4 weeks ago
Science4 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-
 Science4 weeks ago
Science4 weeks agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-
 Science4 weeks ago
Science4 weeks agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment3 months ago
Entertainment3 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









