Health
New Blood Test Promises Faster, Affordable Alzheimer’s Detection

A breakthrough blood test developed by researchers at U.C. San Diego could revolutionize the early detection of Alzheimer’s disease and related dementias. This innovative approach has the potential to significantly reduce both the cost and invasiveness of diagnosis, offering a faster alternative to traditional methods.
The research team identified specific proteins in the blood that increase following brain inflammation and nerve cell damage. These proteins correlate with declines in brain function, suggesting that measuring their levels could provide crucial insights into a patient’s cognitive health. The proposed blood test would analyze these protein surges and compare them against patients’ symptoms, allowing for more timely interventions.
Currently, there is only one approved blood test for Alzheimer’s in the United States, the Lumipulse test, which ranges in cost from $500 to $1,200 and is not typically covered by insurance, according to the Fisher Center for Alzheimer’s Research Foundation. Dr. Freddie Márquez, a postdoctoral scholar at the School of Medicine, emphasized the significance of their findings, stating, “This study highlights the promise of blood-based biomarkers as a more accessible and scalable tool for understanding cognitive decline, particularly in populations that have been underserved by traditional methods.”
Despite the promising results, questions remain about the reliability of using blood tests for large-scale disease detection. Dr. Márquez cautioned that while these tests could enhance a doctor’s diagnosis, they should complement existing diagnostic approaches rather than replace them. “It’s important to note that there’s still a lot we don’t know about the utility of blood-based biomarkers for Alzheimer’s detection,” he said.
Challenges in Current Alzheimer’s Diagnosis
Presently, Alzheimer’s is primarily diagnosed through brain scans that detect specific markers, including the accumulation of toxic proteins. This process can take weeks or even months before a diagnosis is confirmed. Early detection is critical, as it enables patients and their families to plan for the future effectively. Moreover, most treatments for Alzheimer’s are most effective during the early or middle stages of the disease.
The research focused on over 5,700 Hispanic adults aged between 50 and 86 years. This demographic is particularly vulnerable, as Hispanic Americans face a higher risk of developing Alzheimer’s compared to other groups. Factors contributing to this increased risk may include higher prevalence rates of diabetes, stroke, and heart problems among Hispanic populations, which are known to elevate the likelihood of developing Alzheimer’s.
Currently, approximately 7.2 million Americans are living with Alzheimer’s disease, a number expected to rise to nearly 13 million by 2050, driven by the aging population. The ongoing research underscores the urgent need for improved diagnostic tools to address this growing public health challenge.
As scientists continue to explore the potential of blood-based biomarkers, the hope is that these advances will lead to earlier diagnoses and improved care for those affected by Alzheimer’s disease.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science1 month ago
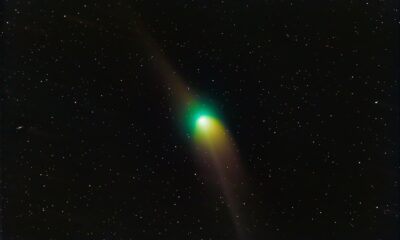
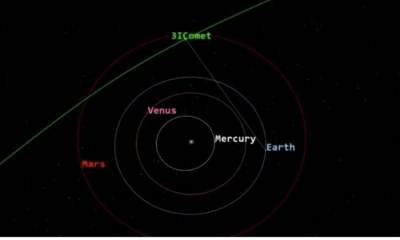
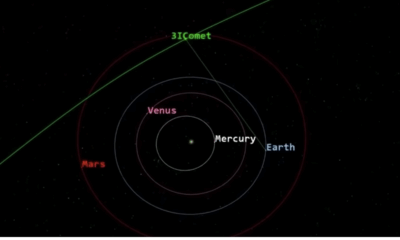
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science1 month ago
Science1 month agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science4 weeks ago
Science4 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science4 weeks ago
Science4 weeks agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-
 Science4 weeks ago
Science4 weeks agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment3 months ago
Entertainment3 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









