Health
NHS Expands Access to Weight Loss Drugs for Diabetes Patients

The National Health Service (NHS) in England is set to significantly expand access to weight loss medications for individuals with type 2 diabetes. This initiative, which marks a major shift in diabetes care, aims to provide earlier access to drugs like Ozempic and other newer treatments, thereby enhancing patient outcomes. The proposed changes come under new guidance from the National Institute for Health and Care Excellence (NICE) and could potentially save nearly 22,000 lives.
In a departure from its previous practices, the NHS is considering a more personalised approach to diabetes treatment. Current guidelines typically place patients on a uniform treatment path, often delaying the introduction of effective medications until later stages of their condition. Under the new recommendations, healthcare providers would be urged to prescribe GLP-1 receptor agonists, such as liraglutide or semaglutide, at the time of diagnosis for patients who also suffer from cardiovascular disease or obesity. This change aims to tackle complications such as heart failure and heart attacks more proactively.
Prof Jonathan Benger, deputy chief executive and chief medical officer at NICE, stated that the guidance would ensure “more people will be offered medicines where it is right to do so.” This shift is expected to greatly benefit an estimated 754,000 patients suffering from cardiovascular disease or early-onset diabetes.
With approximately 4.6 million people in the UK living with diabetes, and an estimated 1.3 million potentially undiagnosed, the implications of these changes are profound. The guidance specifically states that drugs should be considered for diabetes patients who are also diagnosed with heart disease, heart failure, or diagnosed with type 2 diabetes before the age of 40. Additionally, those with a body mass index (BMI) over 35 who have not successfully managed their blood sugar levels within three months of using another medication will also be eligible.
The new recommendations also advocate for the inclusion of SGLT-2 inhibitors, such as canagliflozin and dapagliflozin, as a first-line treatment option for patients unable to tolerate metformin. These medications play a crucial role in managing diabetes by helping the kidneys remove excess glucose from the bloodstream. NICE’s analysis indicated significant under-prescription of these drugs, particularly among women, older adults, and black patients.
Prof Benger remarked, “The evidence from our analysis is clear. There are prescribing gaps that need to be addressed.” The updated guidelines aim to rectify these disparities and enhance access to essential treatments that can help prevent severe health complications.
The proposed changes are currently subject to public consultation, which will remain open until October 2, 2023. Douglas Twenefour, head of clinical at Diabetes UK, expressed optimism regarding the guidelines, noting that they represent a significant evolution in the treatment of type 2 diabetes. He emphasized that improving access to newer treatments will be transformative for patients while ensuring that the UK remains aligned with global advancements in diabetes care.
As the NHS prepares to implement these changes, it also faces challenges related to medication pricing. Earlier this month, concerns emerged over the impending price hike of the weight loss drug Mounjaro, which is expected to nearly double in cost starting from September 1, 2023. Patients have begun scrambling for prescriptions before this increase takes effect, while others are exploring alternatives, including Wegovy, another diabetes medication that has not announced a price rise.
The proposed guidelines underscore the NHS’s commitment to evolving diabetes care, focusing on preventative measures and comprehensive health management. This approach aims to reduce the burden of living with diabetes and address inequities in treatment access and outcomes, ultimately enhancing the quality of life for millions of patients across the UK.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science1 month ago
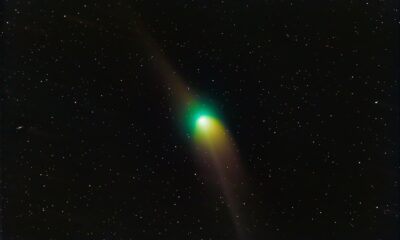
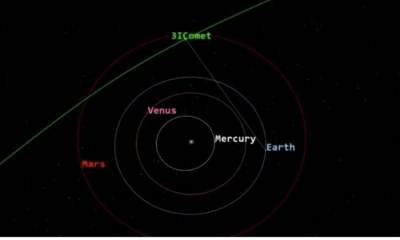
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science1 month ago
Science1 month agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science4 weeks ago
Science4 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science4 weeks ago
Science4 weeks agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-
 Science4 weeks ago
Science4 weeks agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment3 months ago
Entertainment3 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









