Health
Patients Speak Out on Lexapro’s Life-Altering Side Effects

Increasing numbers of patients are raising concerns about the side effects of Lexapro, a widely prescribed antidepressant with nearly nine million users in the United States. Many individuals report that the medication, known generically as escitalopram, has significantly impacted their quality of life, leading some to describe their experiences as “unlivable.”
Sheila Wojciechowski, a 42-year-old mental health counselor from New York, shared her struggles with Lexapro after being prescribed the drug at the age of 21. Initially, she sought treatment following burnout from her job as a special needs teacher and a traumatic breakup. Instead of exploring therapeutic options, her doctor quickly recommended Lexapro. Although she was hesitant, she began taking the medication but felt no improvements after the first week.
In a typical course of treatment, it can take up to eight weeks for patients to experience the full benefits of SSRIs like Lexapro. After reporting her lack of progress to her doctor, Wojciechowski was instructed to increase her dosage from 10 milligrams (mg) to 20 mg per day, which is the highest standard dose recommended. Following this adjustment, she experienced a notable lift in her mood.
Lexapro functions as a selective serotonin reuptake inhibitor (SSRI), which helps increase serotonin levels in the brain, promoting improved mood and reduced anxiety. SSRIs are the most commonly prescribed type of antidepressants, accounting for approximately 70 percent of all antidepressant prescriptions. According to 2024 data, around 11.4 percent of American adults were taking medication for depression, including SSRIs.
During her late 20s, however, Wojciechowski began to notice troubling cognitive side effects, including memory loss and reckless behavior. She described feeling as if she had lost “chunks of time” and remarked on her inability to make sound decisions, leading to risky actions. “I really couldn’t access my compass,” she recalled, acknowledging that she was fortunate to avoid serious consequences during this time.
As the usage of SSRIs continues to rise in the United States, so too does the scrutiny over their side effects. Wojciechowski sought to discontinue Lexapro due to her cognitive concerns but faced challenges in the process. Her doctor recommended a gradual reduction in dosage, as stopping antidepressants abruptly can lead to withdrawal symptoms such as insomnia, nausea, and mood swings.
Despite attempting to taper off, Wojciechowski found that her cognitive symptoms persisted. She described her mental state as chaotic, stating, “My mind just would race and race and race.” She experienced panic attacks and gastrointestinal issues, compelling her to return to Lexapro. This cycle of discontinuation and resumption occurred multiple times over the years, with her longest stretch without antidepressants being 18 months.
To assist with the transition, Wojciechowski was prescribed Wellbutrin, another antidepressant that targets different brain pathways. While Wellbutrin is not an SSRI and works by increasing dopamine and norepinephrine levels, she continued to experience significant anxiety and panic attacks. Ultimately, she reached a breaking point, admitting to suicidal thoughts and agreeing to hospitalization in the summer of 2019.
During her hospital stay, Wojciechowski was diagnosed with psychosis and given a combination of Ativan (lorazepam) and antipsychotic medications. After three months, she switched to a higher dose of Zoloft, another antidepressant, which she reported tolerating better. Yet, when the COVID-19 pandemic struck, her cognitive issues worsened, leading to severe memory problems and emotional instability.
In her quest to manage her symptoms, Wojciechowski adopted a ketogenic diet, which she claims provided some relief. Despite feeling “60 percent better,” she remains cautious about discontinuing her antidepressants. Currently, she is still on Zoloft and reflects on the toll that the medications have taken on her life, including her aspirations of starting a family.
Wojciechowski concluded, “I will not die on these medications, but I’m not tapering anytime soon because I have to work. I have to contribute to my family.” Her story highlights the complex realities faced by many individuals navigating antidepressant use, raising important questions about the balance between treatment and quality of life.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science1 month ago
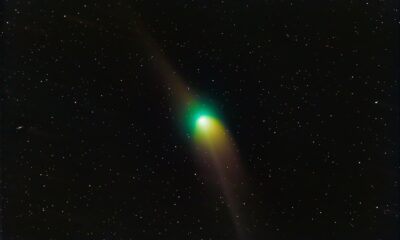
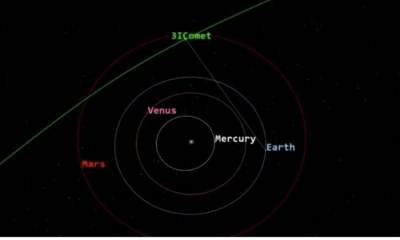
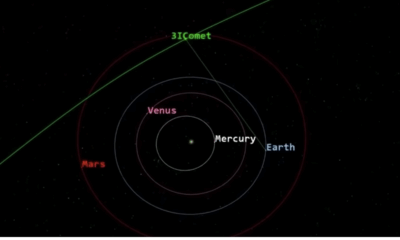
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science1 month ago
Science1 month agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science4 weeks ago
Science4 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science4 weeks ago
Science4 weeks agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-
 Science4 weeks ago
Science4 weeks agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment3 months ago
Entertainment3 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









