Health
Study Reveals Disparities in Diabetes Care Among Racial Groups

The Enhanced Primary Care Diabetes (EPCD) model, designed to improve diabetes care through a nurse-led, multidisciplinary approach, has shown unequal benefits across different racial and ethnic groups. A recent study conducted at Mayo Clinic Rochester analyzed the effectiveness of this model on a diverse patient population, revealing significant disparities in health outcomes.
Researchers examined health records from 1,749 adults, aged between 18 and 75, who participated in the EPCD program from January 1 to December 31, 2020. They followed the patients’ progress until August 1, 2022, focusing on the time it took to achieve five key diabetes care goals, collectively known as the D5. These goals include maintaining a blood pressure reading lower than 140/90, taking a statin to manage cholesterol, achieving an HbA1c level below 8%, remaining tobacco-free, and appropriately using daily aspirin.
During the study, 60.7% of the participants successfully met the D5 goals. However, the findings highlighted a troubling trend: Black patients were significantly less likely to achieve these benchmarks compared to their White counterparts. The hazard ratio for Black patients reaching the D5 was 0.68 (95% CI, 0.52-0.90; P = .007), indicating a discernible gap in care outcomes.
Analysis of Care Engagement
The study further revealed that Asian patients had fewer interactions with nursing staff, averaging only 0.8 nurse touch points per year, while Black patients engaged more frequently, with a median of 2.2 touch points. Hispanic patients did not show a significant difference in care engagement compared to White patients.
Factors contributing to slower attainment of the D5 goals included younger age, insulin use, fewer D5 components met at the outset, and a lower medication count upon entering the program. This suggests that while Black patients were more engaged with care teams, other underlying issues may have impeded their progress in achieving optimal health outcomes.
Implications for Future Care Models
The study’s results emphasize the necessity of tailoring chronic disease management programs to better suit the socioeconomic and cultural contexts of diverse patient populations. The findings have been published in The Annals of Family Medicine by authors from the American Academy of Family Physicians, underscoring the critical need for equitable healthcare solutions.
By addressing these disparities, healthcare systems can improve diabetes care quality for all racial and ethnic groups. This study serves as a call to action for healthcare providers to evaluate their practices and implement strategies that ensure equal access to effective diabetes management.
-

 Health3 months ago
Health3 months agoNeurologist Warns Excessive Use of Supplements Can Harm Brain
-

 Health3 months ago
Health3 months agoFiona Phillips’ Husband Shares Heartfelt Update on Her Alzheimer’s Journey
-

 Science1 month ago
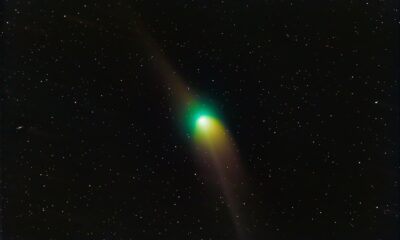
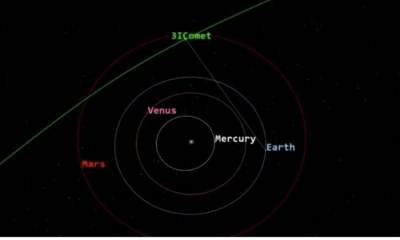
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Science1 month ago
Science1 month agoNASA Investigates Unusual Comet 3I/ATLAS; New Findings Emerge
-
 Science4 weeks ago
Science4 weeks agoScientists Examine 3I/ATLAS: Alien Artifact or Cosmic Oddity?
-

 Entertainment4 months ago
Entertainment4 months agoKerry Katona Discusses Future Baby Plans and Brian McFadden’s Wedding
-
 Science4 weeks ago
Science4 weeks agoNASA Investigates Speedy Object 3I/ATLAS, Sparking Speculation
-

 Entertainment4 months ago
Entertainment4 months agoEmmerdale Faces Tension as Dylan and April’s Lives Hang in the Balance
-

 World3 months ago
World3 months agoCole Palmer’s Cryptic Message to Kobbie Mainoo Following Loan Talks
-
 Science4 weeks ago
Science4 weeks agoNASA Scientists Explore Origins of 3I/ATLAS, a Fast-Moving Visitor
-

 Entertainment4 months ago
Entertainment4 months agoLove Island Star Toni Laite’s Mother Expresses Disappointment Over Coupling Decision
-
 Entertainment3 months ago
Entertainment3 months agoMajor Cast Changes at Coronation Street: Exits and Returns in 2025









